Meta Description:
Explore the gut-brain connection and learn how your microbiome influences mental health, including mood, anxiety, depression, and cognitive function. Find tips to improve gut health for better well-being.
In recent years, one of the most exciting areas of research in health has been the discovery of the powerful link between the gut and the brain—an intricate connection often referred to as the gut-brain axis. While it’s well-established that our brain impacts the gut (think stress-induced stomachaches), emerging science is revealing that the gut may play an equally important role in shaping our mental health. Understanding this gut-brain connection could change the way we approach everything from treating mental health disorders to optimizing cognitive function and overall well-being.
The Microbiome: A Vital Ecosystem
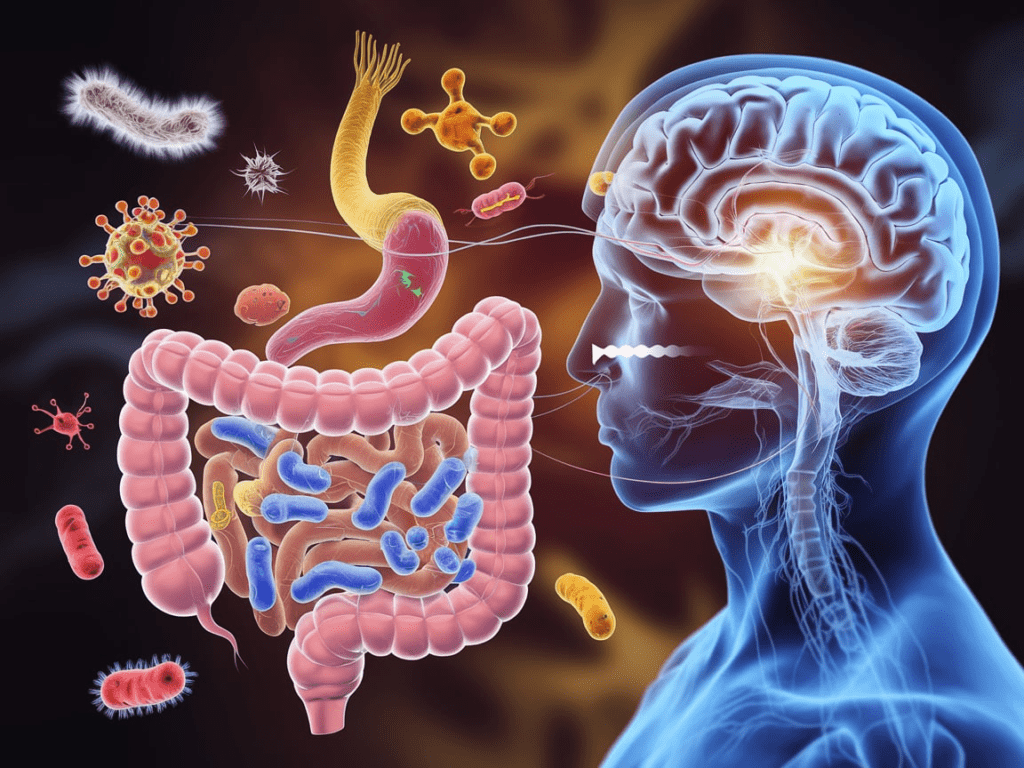
At the heart of the gut-brain connection is the microbiome—the collection of trillions of bacteria, viruses, fungi, and other microorganisms that inhabit our intestines. These microbes are not just passive inhabitants; they are actively involved in a wide range of bodily functions, including digestion, immune system regulation, and even hormone production. The gut microbiome is a complex ecosystem, and its balance or imbalance can have a profound effect on physical and mental health.
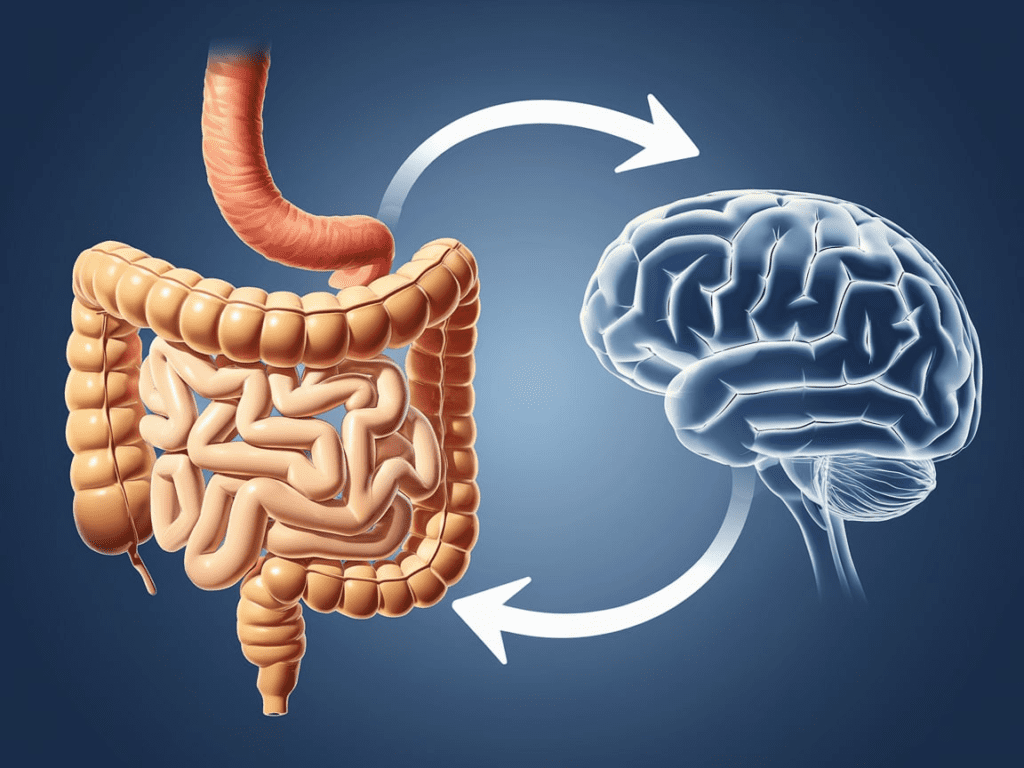
Interestingly, the microbes in our gut are able to communicate with the brain through several pathways, such as via the vagus nerve (which runs from the brainstem to the abdomen) and through the production of various neurotransmitters and other bioactive compounds. This bidirectional communication between the gut and the brain is a key component in understanding how our mental state can be influenced by gut health.
The Gut-Brain Axis: How It Works
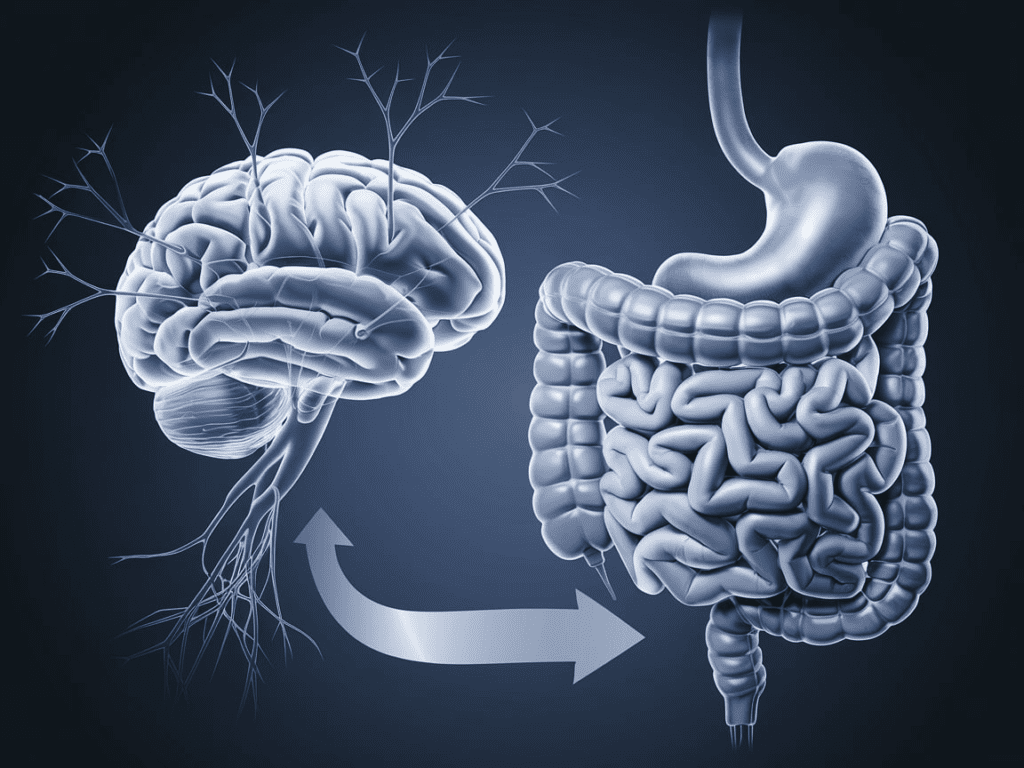
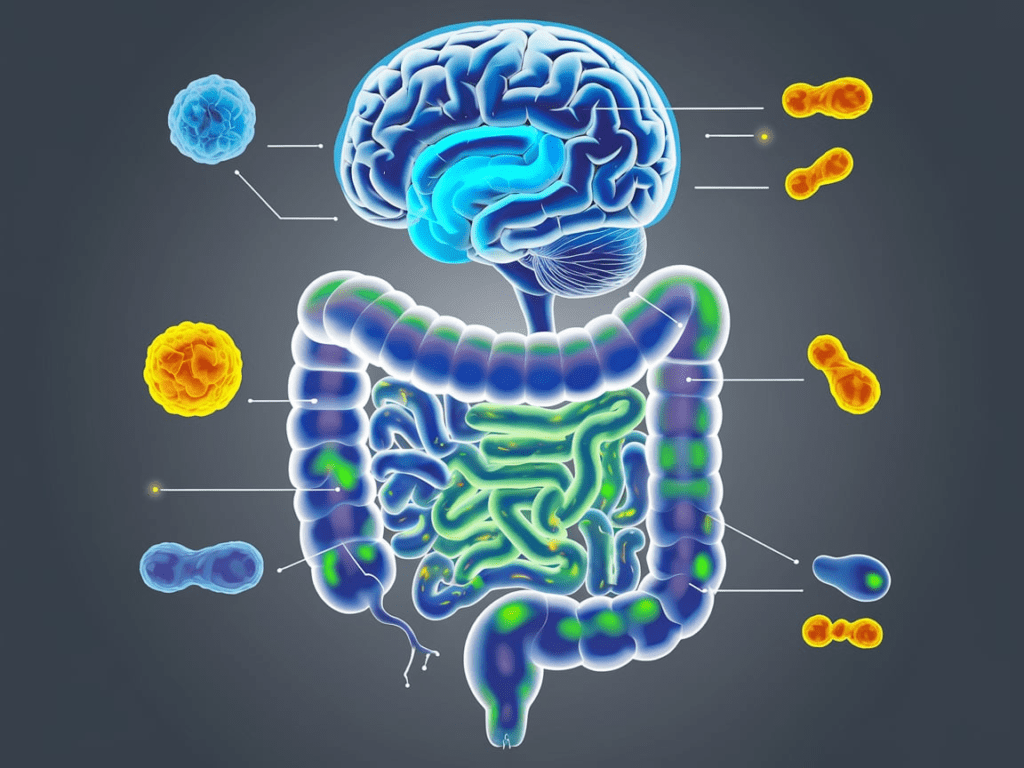
The gut-brain axis refers to the complex signaling network that connects the gut microbiome with the central nervous system (CNS). This communication happens in a variety of ways:
- Neurotransmitters and Hormones: Many of the chemicals responsible for mood regulation are produced in the gut. For example, approximately 90% of serotonin, a neurotransmitter often referred to as the “feel-good” hormone, is produced in the gut. Disruptions in the microbiome can affect serotonin levels, potentially influencing mood disorders such as anxiety and depression.
- Immune System Interaction: The gut microbiome plays a major role in regulating the immune system. An imbalance in gut bacteria (often called dysbiosis) can lead to systemic inflammation, which has been linked to mental health issues like depression and anxiety. Inflammation in the brain, driven by immune responses in the gut, can contribute to cognitive and mood disturbances.
- Short-Chain Fatty Acids (SCFAs): These byproducts of microbial fermentation have been shown to promote brain health. SCFAs can influence brain function by modulating gene expression and reducing inflammation. They help to support the blood-brain barrier, protecting the brain from harmful substances.
- The Vagus Nerve: The vagus nerve, a major pathway of communication between the gut and the brain, allows signals from the gut to influence brain activity. The vagus nerve plays a role in regulating mood, stress responses, and cognition, and it’s thought that changes in gut microbiota composition may impact vagus nerve signaling.
The Impact of the Gut Microbiome on Mental Health
Research on the microbiome’s influence on mental health is still in its early stages, but some studies suggest that gut health plays a critical role in a variety of psychiatric conditions:
- Depression and Anxiety: Imbalances in gut bacteria have been linked to both anxiety and depression. A reduced diversity of gut microbes has been associated with increased risk for these mood disorders. Additionally, probiotic and prebiotic interventions—methods that promote healthy gut bacteria—have shown promise in alleviating symptoms of depression and anxiety.
- Autism Spectrum Disorder (ASD): Some studies suggest that children with ASD have distinct microbiome profiles compared to neurotypical children. While the exact mechanisms remain unclear, there is growing interest in exploring how altering the microbiome might help manage symptoms of ASD.
- Cognitive Function: The gut microbiome also appears to influence cognitive function. Some research has suggested that gut bacteria can influence brain development, memory, and learning abilities. Imbalances in gut microbes may contribute to neurodegenerative diseases like Alzheimer’s.
- Stress Response: Chronic stress can disrupt the microbiome, leading to a vicious cycle of gut-brain communication that worsens stress and anxiety. However, certain dietary and lifestyle changes that improve gut health may help break this cycle and improve stress resilience.
Supporting Gut Health for Better Mental Health
While much of the research is still ongoing, there are several ways to support your gut microbiome for potential mental health benefits:
- Eat a Diverse, Plant-Based Diet: A diet rich in fiber, fruits, vegetables, and whole grains supports a healthy, diverse microbiome. These foods provide the prebiotics (non-digestible fibers) that nourish beneficial gut bacteria.
- Probiotics and Fermented Foods: Adding probiotics through supplements or fermented foods (such as yogurt, kefir, sauerkraut, and kimchi) may help maintain a healthy gut microbiome.
- Manage Stress: Since chronic stress can negatively affect gut health, incorporating stress-management techniques such as mindfulness meditation, yoga, and regular physical activity can help maintain both mental and gut health.
- Avoid Unnecessary Antibiotics: Overuse of antibiotics can disrupt the balance of the microbiome, leading to dysbiosis. Use antibiotics only when prescribed by a healthcare professional and always complete the prescribed course.
- Sleep Well: Quality sleep is crucial for maintaining gut health. The microbiome functions better when the body is well-rested, as sleep influences the production of beneficial gut metabolites.
Conclusion
The gut-brain connection is a groundbreaking area of research that has the potential to revolutionize how we approach mental health. While more research is needed to fully understand the complexities of this connection, early findings suggest that maintaining a healthy microbiome could be key to improving mental well-being. By focusing on a balanced diet, stress management, and overall wellness, you can take proactive steps to support both your gut and your brain, leading to better mental health outcomes.
Frequently Asked Questions (FAQs)
1. How does the gut influence mental health?
The gut influences mental health through the production of neurotransmitters, immune system regulation, and communication with the brain via the vagus nerve. Imbalances in the gut microbiome can contribute to mental health conditions such as anxiety, depression, and stress.
2. Can improving gut health reduce anxiety or depression?
Yes, studies suggest that improving gut health through diet, probiotics, and lifestyle changes can help alleviate symptoms of anxiety and depression by balancing gut bacteria and reducing inflammation.
3. What are some foods that support a healthy gut microbiome?
Foods rich in fiber, such as fruits, vegetables, legumes, and whole grains, as well as fermented foods like yogurt, kefir, and kimchi, support gut health by nourishing beneficial bacteria.
4. Can probiotics help with mental health?
Some research indicates that probiotics, which are beneficial bacteria, may improve mood and reduce symptoms of depression and anxiety by supporting a healthy gut microbiome.
5. Is there a link between gut health and autism?
Some studies suggest children with autism spectrum disorder (ASD) have distinct gut microbiomes compared to neurotypical children, though more research is needed to understand the potential impact of the microbiome on ASD symptoms.